You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Replacing natural teeth with dental implants instead of conventional treatment modalities has become commonplace in the contemporary surgical and restorative practice. Their use has been well documented in the dental literature.1,2 Furthermore, with advancements in surgical techniques and implant designs, their efficient use in the esthetic zone has become a successful and predictable tooth replacement option, and the most conservative approach when the adjacent natural teeth are untouched.3-7
Occasionally, tooth replacement procedures with dental implants do face some compromised circumstances, which can cause the more conventional implant sizes (diameters) to not be usable.8-12 Smaller edentulous intertooth spaces, reduced vertical or transverse dimension of the residual ridge, convergent roots, and/or close proximity of root trunks can lead to the implant team to forego the implant process for more conventional methods of tooth replacement. Another common deterrent to the use of dental implants is the compromised edentulous space remaining in the congenitally missing lateral incisor area of the maxillary anterior, either pre- or post-orthodontic treatment. Traditionally, this type of edentulous space was forced to be restored with a removable type appliance or some type of resin-bonded bridge.
In the extreme, treatment of these compromised areas may also lead to full-coverage restorations of the abutment teeth, with a fixed pontic to replace the edentulous space. In adolescent adults and younger individuals, this can lead to significant reduction of the natural teeth adjacent to the edentulous space that otherwise would remain untouched for many years to follow. This may lead to future endodontic procedures, multiple replacements of crowns and/or bridges over the patient’s lifetime, and possibly premature tooth loss. Additionally, a compromised esthetic result is usually obtained as a result of the insufficient tooth-to-tooth space.11-14
To properly create an ovate pontic emergence profile in the soft tissue, which is necessary to provide for a natural-appearing pontic in the fixed bridge tooth replacement option, certain considerations must be discussed when replacing the congenitally missing or compromised intertooth edentulous space. Criteria of the routine implant site require that a normal two-piece implant be placed at least 1.5 mm from the adjacent teeth.12-14 As such, the width of an edentulous space that will receive a normal two-piece dental implant should be at least 6.5 mm wide, taking into consideration 1.5 mm from the adjacent teeth and the implant diameter being 3.5 mm; 7.5 mm if the implant diameter is 4.5 mm; and 8.5 mm if the implant diameter is 5.5 mm. Additionally, the implant team must take into consideration that the width of the abutment is usually greater than the implant itself, which leads to the proper emergence profile formation of the soft tissues supporting the planned final restoration. Therefore, the minimum intertooth space must be increase by at least 1 mm to accommodate the final restoration.
As a result of the aforementioned measurements, larger-diameter implants cannot be used to treat these compromised sites. Small-diameter implants are ideal for sites that are insufficient, and various designs have been reported on in the literature over the last 15 plus years.15-22 Manufacturers have provided small-diameter implants ranging in diameter from 1.8 mm to 3.3 mm in width, and 8 mm to 16 mm in length. Their use in implant treatment has ranged from immediate stabilization of bone-augmented ridges to esthetic tooth replacement in the esthetic zone.
The following outlines the author’s clinical application for narrow-diameter, one-piece implants (1.8 mm to 3 mm):
- Immediate loading of a provisional appliance
- Orthodontic anchorage
- Immediate full-arch edentulous denture stabilization
- Single-tooth replacement, compromised intertooth space
- Cases requiring minimally invasive surgical procedures (ie, health concerns, residual ridge deficiencies, advanced oral infections)
- Management of congenitally missing natural teeth
- Management of mandibular central and lateral incisors
Continued expansion of their use has also led to design feature changes and advancements, and because of compromised intertooth width and resultant emergence profile formation issues, the one-piece implant design has become more accepted as a tooth replacement option in these types of cases. Implant systems that incorporate the abutment as part of the implant itself do not have a “gap” between the implant body and abutment connection, and, therefore, bone loss over time may be reduced with their use. The reduction in the diameter of the crestal portion of the one-piece design allows for crucial millimeters of space to be conserved in the compromised intertooth space which, when used to replace the natural tooth system in the esthetic zone, can be a critical factor in the esthetic result obtained in the compromised site.
The following case report will demonstrate the use of small-diameter, one-piece implants being used to correct edentulous sites remaining from congenitally missing maxillary lateral incisor teeth.
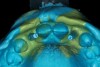
A 19-year-old non-smoking female presented for tooth replacement at the maxillary right and left lateral incisors, which were congenitally missing (Figure 1). The post-orthodontic result was adequate for the placement of 3-mm one-piece small-diameter implants. The preoperative radiographs can be seen in Figure 2 and Figure 3. The pretreatment clinical view in Figure 4 and Figure 5 shows the small intertooth space present in the lateral incisor areas. One of the most challenging tasks with congenitally missing lateral incisor cases is to create an acceptable soft tissue emergence profile from a crestal profile that is flat from the mesial of the canines to the distal of the centrals (Figure 4 and Figure 5). After pretreatment planning which consisted of a complete medical and dental history, radiographic analysis, and upper and lower study models mounted by a facebow transfer technique, the fabrication of a TempStent II surgical guide was completed. Figure 6 and Figure 7 show the occlusal view of the TempStent II guide on the study cast and in the oral cavity, respectively.
After administration of an appropriate local anesthetic and prior to initial coring of the implant surgical site, procedures were completed to ensure proper implant positioning and creation of the esthetic tissue emergence profile in the crest of the ridge. This was completed by placement of the TempStent II (Figure 8) and then through the occlusal aspect of the surgical guide, marking the crest of the ridge with a #8 round diamond. Once this was completed, creation of the soft tissue emergence profile was then accomplished by placing a football-shaped diamond into the high-speed handpiece, and then outlining the soft tissue to follow the flow of the emergence profile of the canine to the central, outlining the emergence profile of the lateral site, and creating interproximal papillary contours. This shaping of the gingival tissues was then continued to the osseous crest, and the same dimension was carried on to the alveolar structures, thereby taking the biologic width into account. This allowed for a sculpted implant receptacle site for the minimally invasive surgical approach for implant placement. Assessment of the width of attached gingiva should be performed prior to this procedure to ensure that an adequate band will be present at the conclusion. If an inadequate width will remain after coring the site, then a crestal incision and displacement of the keratinized gingiva facially may be a better approach. Based on pre-surgical evaluation, the buccal/palatal dimension of the edentulous ridge was acceptable for this minimally invasive approach, and the minimal amount of bone grafting required to “plump” the facial aspect of the site was easily accomplished by a “pouch” grafting technique to enhance the cosmetic aspect of the case.
After atraumatic site preparation, two 3-mm diameter by 10-mm in length one-piece implants were seated at the No. 7 and No. 10 sites (Zimmer Dental, Carlsbad, CA) (Figure 9). Note the emergence profile formed by the esthetic recontouring of the crest of the ridge prior to implant site preparation. Confirmation of implant positioning was then verified by placing the TempStent II guide over the surgical sites (Figure 10). Ideally, because the heads of these implants are not wide and they do not lend themselves to gross preparation to reduce the facial aspect, the implants may not be suited for maxilla that has a steep angle. Minor preparation of the head can be performed facially but should be kept to a minimum.
Reconstruction of the facial aspect of the surgical site was completed by the conservative “pouch” technique. Creation of a contained space on the facial aspect of the implant site allowed for the placement of a mineralized cancellous graft complex to build the facial aspect of the implant site (Figure 11). The graft complex consisted of mineralized cancellous chips 1 µm to 2 µm particle size (LifeNet, Salvin Dental, Charlotte, NC) and a demineralized freeze-dried bone allograft (Regenafil, Exactech, Inc, Gainesville, FL) to create a putty-type consistency. Figure 11 shows the “plumping” of the facial aspect of the implant site.
Conversion of the surgical guide to the esthetic provisional was then completed by retrofitting the surgical guide with restorative composite, and then placing the guide back over the provisional copings that were seated on the abutment portion of the one-piece implants, and curing the surgical guide with a curing light (Figure 12). The guide was then reviewed, with the provisionals in the guide, then removal of the provisionals from the vacuform portion of the guide allowed for correction of the marginal portion of the provisionals using a flowable composite material. Shaping the line angles and emergence profile of the provisionals allowed for the proper contours of the provisional to be accomplished (Figure 13). The provisionals were then cemented with a strong temporary cement. The immediate postoperative clinical view can be seen in Figure 14 and Figure 15. The provisionals were immediate, non-functional restorations in centric occlusion and relation, and lateral right and left excursive movements. Figure 16 and Figure 17 show the immediate postoperative radiographic view. Note how the 3-mm diameter implant allows for the adequate space between the root surfaces and the implants placed.
The 3-month postoperative views can be seen in Figure 18 through Figure 20. Note the excellent soft tissue emergence profiles obtained from the properly contoured provisional restorations. After removal of the provisional restorations, further inspection of the contoured emergence profile obtained has been accomplished (Figure 21 and Figure 22). Before impression techniques, transfer copings were seated over the abutment portion of the one-piece implant (Figure 23). A full-arch impression was then taken using medium-body impression material (Take 1 Advanced, Kerr Corporation, Orange, CA) and a regular-body wash material (Take 1 Advanced) to pick up the detail of the emergence profile and impression coping (Figure 24 through Figure 26). After allowing the impression material to set, the impression is then removed from the mouth and inspected (Figure 27). The Take 1 Advanced Medium body has a more rigid set than most other medium materials, so when the coping is placed back in the impression, the possibility of movement during casting is reduced. Please note how the emergence profile obtained has been registered in the impression, and can easily be transferred to the laboratory technician. Laboratory analogues are then placed into the impression coping and forwarded to the laboratory technician for pouring of the casts and final fabrication of the esthetic implant restorations (Figure 28).
Conclusion
Management of compromised intertooth spaces presents a difficult challenge for the dental implant team. Often times an edentulous space is less than 5 mm from tooth-tooth, this space is usually in the esthetic zone, and the implant team is expected to develop proper soft tissue architecture and emergence profiles when conventional parameters of esthetic implantology do not apply. These challenged spaces present limits on how they are handled and require implants that are 3-mm in diameter or less. Incorporating smaller-diameter implants into treatment protocols provides patients who normally would not be able to proceed with implant reconstruction to have dental implants, and replace the natural tooth system without having to damage the adjacent natural teeth. Proper placement and restorative techniques can lead to esthetic results, with natural-appearing soft tissue contours and emergence profile formations that mimic the natural tooth that was replaced.
References
1. Branemark P-I, Zarb GA, Albrektson T, eds. Tissue-Integrated Prosthesis: Osseointegration in Clinical Dentistry. Carol Stream, IL: Quintessence Publishing: 1985:11-81.
2. Adell R, Lekholm U, Rockler B, et al. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
3. Kan JY, Rungcharassaeng K. Immediate placement and provisionalization of maxillary anterior single implants: A surgical and prosthetic rationale. Pract Periodontics Aesthet Dent. 2000;12:817-824.
4. Saadoun AP. Immediate implant placement and temporization in extraction and healing sites. Compend Contin Educ Dent. 2002;23:309-323.
5. Petrungaro PS. Immediate implant placement and provisionalization in edentulous, extraction and sinus grafted sites. Compend Contin Educ Dent. 2003;24:95-113.
6. Petrungaro PS. Immediate restoration of implants utilizing a flapless approach to preserve interdental contours. Pract Proced Aesthet Dent. 2005;17:151-158.
7. Wohrle PS. Single-tooth replacement in the aesthetic zone with immediate provisionalization: fourteen consecutive case reports. Pract Periodontics Aesthet Dent. 1998; 10:1107-1114.
8. Thompson VP, deRijik KW. Clinical evaluation and lifetime predictions for resin-bonded prosthesis. In: Anusavice KJ, ed. Quality Evaluation of Dental Restorations; Criteria for Placement and Replacement of the International Symposium for Place. Chicago, IL Quintessence. 1989:373-386.
9. Hansson O. Clinical results with resin-bonded prostheses and an adhesive cement. Quintessence Int. 1994:25:125-132.
10. Shugars Da, Bader JD, White BA, et al. Survival rates of teeth adjacent to treated and untreated posterior bounded edentulous spaces. J Am Dent Assoc. 1998;129:1089-1098.
11. Wallace SS. Significance of the “biologic width” with respect to root form implants. Dent Implantol Update. 1994;5:25-29.
12. Misch CE. Early bone loss etiology and its effect on treatment planning. Dent Today. 1996;15:44-51.
13. Salama H, Salama M, Garber D, et al. Developing optimal peri-implant papillae within the esthetic zone: guided soft tissue augmentation. J Esthet Dent. 1996;8:12-19.
14. Misch CE. Treatment options for a congenitally missing lateral incisor. A case report. Dentistry Today. 2004;23(8):92-95.
15. Petrungaro PS. Fixed temporization and bone augmented ridge stabilization with transitional implants. Pract Periodontics Aesthet Dent. 1997;9(9):1071-1078.
16. Froum S, Emtiaz S, Bloom MJ, et al. The use of transitional implant for immediate fixed temporary prosthesis in cases of implant restorations. Pract Periodontics Aesthet Dent. 1998; 10(6):737-746.
17. Babbush CA. Dental Implants: The Art and Science. Philadelphia, PA: WB Saunders Co. 2001:201-216.
18. Andersson B, Odman P, Lindvall AM, Lithner B. Single tooth restorations supported by osseointegrated implants: results and experiences from a prospective study after 2 to 3 years. Int J Oral Maxillo Imp. 1995;10:702-710.
19. Anderson B, Saxegaard E, Knutson BM, Haanaes HR. A prospective clinical study evaluating the safety and effectiveness of narrow-diameter threaded implants in the anterior region of the maxilla. Int J Oral Maxillo Imp. 2001;16:217-224.
20. Davarpanah M, Martinez H, Tecuelanu JP, et al. Small diameter implants: indications and contraindications. J Esthet Dent. 2000;12:186-194.
21. Block MS, Delgado A, Fontenot MG. The effect of diameter and length of hydroxyzilapatite-coated dental implants on ultimate pullout force in dog alveolar bone. J Oral Maxillofac Surg. 1990;48:174-178.
22. Lazzara RJ, Siddiqui AA, Binon P, et al. Retrospective multicenter analysis of 3i endosseous dental implants placed over a five-year period. Clin Oral Impl Res. 1996;7:73-83.